About the author:
Chris Boyd is general manager of building water health for NSF International. Boyd can be reached at [email protected].
The number of Legionnaires’ disease cases reported to the U.S. Centers for Disease Control and Prevention (CDC) increased more than eight fold between 2000 and 2018 to a record 9,933 cases. Further, we know the disease is largely underreported. In its extensive report, Management of Legionella in Water Systems, published Aug. 14, 2019, the National Academies of Sciences, Engineering, and Medicine conservatively estimated 52,000 to 70,000 people contract Legionnaires’ disease annually in the U.S.
Identifying Locations At Risk
When evaluating where Legionella outbreaks occur, the CDC found 33% of all building-associated Legionella outbreaks occurred in a healthcare setting, 25% of healthcare-acquired Legionnaires’ disease cases are fatal and nine out of 10 outbreaks could have been prevented had a properly designed water management plan been implemented.
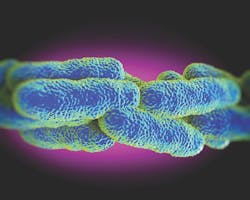
Legionnaires’ disease is a severe pneumonia-like illness caused by inhaling Legionella bacteria. People who are immunocompromised are among those most at risk. According to the American Hospital Association, nearly 37 million people are admitted to hospitals every year in the U.S., so implementing a comprehensive water management plan for hospitals and health facilities is critical.
Recognizing the importance of preventing Legionnaires’ disease in healthcare settings, the federal Centers for Medicare & Medicaid Services (CMS) took an important step in 2017 by requiring all hospitals, long-term care centers and skilled nursing homes to perform an environmental assessment of their water systems, develop a water management program and establish sampling and monitoring strategies for each of their facilities.
Preventing Legionella cases requires understanding how risks are amplified. Legionella poses no significant public health risk in its natural environment in rivers, lakes and streams. It becomes a public health risk when it enters warm, low-flowing or stagnant water plumbing systems that allow it to amplify and then disperse into the environment through aerosolized droplets that can be inhaled. Common sources of contaminated mists are showers, hot tubs, decorative fountains and cooling towers.
Creating a Water Management Plan
In a healthcare environment, the water management plan needs to cover those common sources of exposure, as well as dozens of other potential hazards that are unique to healthcare facilities. From hydrotherapy units and heater-cooler devices to respiratory care devices and dental or surgical water lines, hospitals and long-term care facilities contain many water applications that must be incorporated into the water management plan. Additionally, healthcare facilities need to manage risk in complex and diverse settings—from burn centers, oncology units, neo-natal ICUs and surgical theaters—as each have unique water systems and exposure risks that must be evaluated and controlled.
Approaching the management of risk in a complex healthcare environment requires individualized assessments of each facility. Effective healthcare water management plans include a multidisciplinary team consisting of senior leadership, facility engineering, biomedical engineering, infection prevention, nursing and vendors that have been charged with routine maintenance. The healthcare facility management team must work together to perform an environmental assessment of the entire facility, identifying areas of high risk due to patient populations and the presence of hazardous conditions. It is important to walk the facility and not to rely on engineering drawings.
Building on an individualized, site-specific risk assessment and reviewing the existing procedures, such as device manufacturers’ operating requirements, the team should develop a water management program that defines specific actions to control risks. The team must communicate regularly on the implementation of the program to ensure all actions are performed according to the established procedures. Documentation of these actions is essential to verify the program is being implemented as designed and for the team to be able to review the effectiveness of the program on an ongoing basis.
While it may seem daunting to develop a comprehensive water management plan for facilities with complex systems, the reality is that many of the cleaning, disinfection and monitoring activities required are already being performed. The water management plan will identify gaps in current practices and provide transparency across different departments on their efforts. It also will help the facility develop a coordinated policy for how risks are being managed and ensure all stakeholders in patient safety support the creation of a positive water safety culture that will prevent avoidable illnesses and deaths.
Developing consistent strategies to prevent Legionella growth in healthcare settings emerged as a key challenge at the recent Legionella Conference 2019, co-presented by NSF International and the National Environmental Health Association in Los Angeles and will be a primary focus of next year’s conference hosted in Chicago.